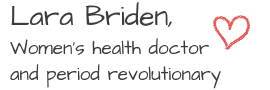
Polycystic ovary syndrome (PCOS) is not one disease. Instead, it’s “a heterogeneous disorder with different underlying biological mechanisms.” In other words, it’s a set of symptoms (androgen excess and anovulatory cycles) caused or driven by several underlying factors. To successfully treat PCOS, you need to identify which factor (or factors) is driving the symptoms. In other words, you need to know your functional type of PCOS.
The four functional types of PCOS include insulin-resistant PCOS, post-pill PCOS (which is temporary), inflammatory PCOS, and the far less common adrenal PCOS.
First things first, what is PCOS?
PCOS is best defined as androgen excess (high male hormones) when all other causes of androgen excess have been ruled out. And despite the name, polycystic ovary syndrome has nothing to do with cysts on the ovaries. For one thing, the so-called “cysts” visible on ultrasound are not ovarian cysts but are just follicles or eggs, which are normal for the ovary.
💡Tip: Large, abnormal ovarian cysts can cause pain and other symptoms. They are separate issues and not the same thing as polycystic ovaries.
For another thing, “there is no evidence that the presence of polycystic ovaries has any implications with regard to the endocrine or metabolic features of PCOS.” In other words, you can have polycystic ovaries and have perfectly normal hormones. Conversely, you can have normal-looking ovaries but still have the hormonal condition of androgen excess (aka PCOS).
So, the first step in determining your type of PCOS is to ask the question, “Is it really PCOS? “
Is it really PCOS?
It’s PCOS if you have androgen excess, as demonstrated by 1) high androgens (male hormones) measurable on a blood test and/or 2) significant facial hair or jawline acne. Plus, other reasons for androgen excess have been ruled out.
💡Tip: Other reasons for androgen excess include congenital adrenal hyperplasia (which accounts for up to 9 percent of cases of androgen excess), high prolactin, and hormonal birth control with a high androgen index (testosterone-like progestin).
If you don’t have androgen excess, then you don’t have PCOS. That’s true even if you have polycystic ovaries, and that’s true even if you have irregular periods or no periods. There are lots of reasons for no periods, including the very common hypothalamic amenorrhea, which is a lack of periods due to undereating or undereating carbs. (And yes, you could have been mistakenly told you have “lean PCOS” when you actually have hypothalamic amenorrhea.)
For more information, read:
- PCOS cannot be diagnosed (or ruled out) by ultrasound
- Pain is not a symptom of PCOS
- Is it PCOS or hypothalamic amenorrhea or both?
If you’re certain you have PCOS, let’s move on. Do you have insulin resistance?
Insulin-resistant PCOS
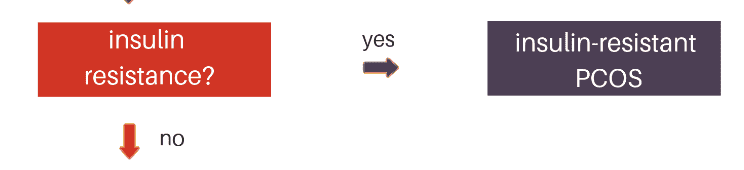
Insulin resistance means having high insulin. It’s also called metabolic syndrome or pre-diabetes. The best way to test for insulin resistance is to measure the hormone insulin, not glucose.
💡Tip: For more information about insulin testing, see my book Metabolism Repair for Women.
If your insulin is high, then high insulin is driving your high androgens, and you have insulin-resistant PCOS.
The treatment of insulin-resistant PCOS is to reverse insulin resistance with all the strategies I discuss in my new book about insulin resistance.
💡Tip: There’s a 70 percent chance your PCOS is insulin-resistant PCOS.
If you’re certain you do not have insulin resistance, let’s move on. Did your symptoms start when coming off the pill?
Post-pill PCOS
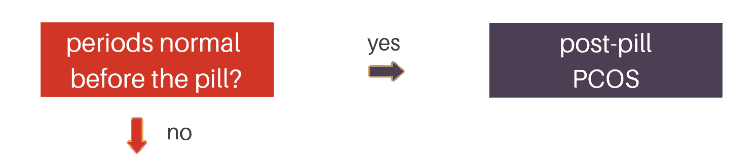
It’s pretty common to experience a temporary surge in androgens when coming off drospirenone or cyproterone pills like Yasmin, Yaz, Diane, or Brenda. Under current diagnostic guidelines, that temporary surge in androgens is enough to qualify for the diagnosis of PCOS or post-pill PCOS.
For more information, read, watch, or listen to Help for post-pill acne, hair loss, and weight gain.
You have post-pill PCOS if you meet the criteria for PCOS (excess androgen and other conditions ruled out), plus you do not have insulin resistance, plus symptoms started when trying to come off the pill.
If you did not just come off the pill (or spironolactone) or had problems before birth control, let’s move on. Do you have signs of chronic inflammation?
Inflammatory PCOS

Chronic inflammation can stimulate the ovaries to make too much testosterone and is a factor in every type of PCOS.
When chronic inflammation is the primary factor or driver, it’s inflammatory PCOS.
The treatment for inflammatory PCOS is to identify and correct the underlying source of inflammation. That could mean avoiding food sensitivities such as dairy, fixing an underlying gut problem, or addressing chronic mast cell activation or histamine intolerance. The supplements zinc and N-acetyl cysteine work particularly well for inflammatory PCOS.
You have inflammatory PCOS if you meet the criteria for PCOS, plus you do not have insulin resistance, plus you’re not in a temporary post-pill phase, plus you have signs and symptoms of inflammation, as follows:
- unexplained fatigue
- bowel problems like IBS or SIBO
- autoimmune disease like Hashimoto’s thyroid disease
- headaches
- joint pain
- a chronic skin condition like psoriasis, eczema, or hives.
If you do not have chronic inflammation, let’s move on. Do you have adrenal PCOS?
Adrenal PCOS
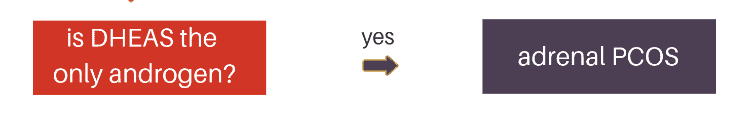
Most women with PCOS have an elevation of all androgens, including testosterone and androstenedione from the ovaries and DHEAS from the adrenal glands.
If you have only elevated DHEAS (but normal testosterone and androstenedione), you may have adrenal PCOS, which accounts for 10 percent of PCOS cases. Adrenal PCOS is similar to the genetic condition late-onset congenital adrenal hyperplasia (CAH).
Adrenal PCOS is not driven by insulin resistance or inflammation. Instead, it’s an epigenetic upregulation of adrenal androgens. Treatments include magnesium, zinc, licorice, adaptogen herbs, and pantothenic acid (vitamin B5), which modulates adrenocorticotropic hormone (ACTH).
💡 Tip: What if you have more than one type? The types are listed in order of priority. So, if you have insulin resistance, then you have insulin-resistant PCOS—even if you also have inflammation and a post-pill worsening of your symptoms.
Anti-androgen treatment for all types
In addition to treating the underlying driver of your PCOS, you may also require a natural anti-androgen supplement such as cyclic progesterone therapy.
Still confused?
What if you’ve been told you have PCOS but don’t meet any of the above criteria?
Go back to the drawing board. Do you truly have PCOS? As in, do you have high androgens? If not, you don’t have PCOS and could instead have hypothalamic amenorrhea.
See the full flowchart below and ask me in the comments. For information about the four types of PCOS and their treatments, see Chapter 7 of Period Repair Manual.