
What do post-pill acne, hair loss, and weight gain all have in common? They can all be the result of a temporary surge in androgens when trying to come off certain types of hormonal birth control.
In episode eight of my podcast/YouTube video, I discuss post-pill androgen symptoms including why pills like Yasmin are the hardest to come off, how androgens can cause weight gain, and natural treatments such as zinc, berberine, and cyclic progesterone therapy.
Also available wherever you get your podcasts.
Transcript
What do post-pill acne, hair loss, and weight gain all have in common? Well, they can all be the result of a temporary surge in androgens when trying to come off certain types of hormonal birth control.
Welcome back to the podcast. I’m your host Lara Briden, a naturopathic doctor and author of the books Period Repair Manual and Hormone Repair Manual.
I live in New Zealand but am currently in Southern Alberta, Canada visiting family and going on lots of walks. I’m also away from my good mic. So, if today’s audio quality is not as good as other episodes, that’s why. It’s the summer holiday episode.
As promised, today is all about post-pill androgen symptoms such as acne, hair loss, and weight gain.
They’re androgen symptoms because they’re caused by the temporary surge in testosterone or other androgens or male hormones that can occur when stopping a combined estrogen method of hormonal birth control, especially one that contains an anti-androgen progestin like drospirenone or cyproterone. A classic example is the acne when trying to come off Yas or Yasmin, but certain other pills can cause similar issues.
I say “temporary” surge in androgens, but in actual fact, symptoms can persist for a couple of years which can feel like a really long time when you’re struggling with the worst breakouts you’ve ever had. And unfortunately, a couple of years of post-pill androgen symptoms can easily lead to a somewhat questionable PCOS diagnosis. That’s the temporary post-pill PCOS that I discuss in my book and on my blog.
Which is not to say you can’t legitimately have PCOS when coming off the pill—you can. But in that case, you’re likely to have had at least some androgen symptoms before you went on the pill. For more about PCOS and why it cannot be diagnosed by ultrasound, check out episode 3 of the podcast.
For now, let’s focus on the temporary post-pill androgen surge and what you can do about it. Keeping in mind, this concept of “post-pill androgen surge” applies only when you’re coming off synthetic estrogen and/or an anti-androgen progestin like drospirenone. If you’re coming off a pro-androgen progestin like levonorgestrel in the hormonal IUD, for example, you should find your skin and weight improve.
And just to be clear, androgen excess can be diagnosed by blood test and/or symptoms. In other words, if you have androgen symptoms like facial hair or strong jawline acne, then you have high androgens, even if your testosterone is normal on a blood test.
And if you’re puzzled that I keep mentioning weight gain as an androgen symptom. Yes. In women, androgen excess can cause insulin resistance and weight gain around the middle. In men, it’s the complete opposite. In men, a higher level of testosterone can promote healthy insulin sensitivity and weight loss around the middle. The tendency of androgens to promote weight gain in women is why progestins with a high androgen index (such as levonorgestrel) can cause weight gain. While progestins with a very low androgen index (such as drospirenone) can cause weight loss for as long as you take them. But then rebound weight gain when you try to stop them. The topic of today.
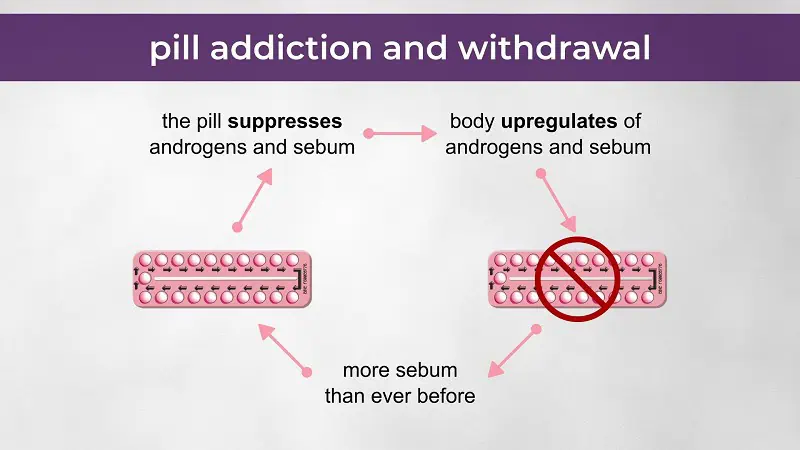
Now. If you’re suffering with post-pill androgen symptoms, please know it’s not necessarily a problem with you, but with the medication you’re trying to withdraw from. Think of it this way. You had a baseline level of androgens and skin oils or sebum. But then, when you started the pill, the synthetic estrogen and drospirenone suppressed both androgens and sebum, which would have cleared up your skin, and possibly promoted weight loss. At that point, your androgens and sebum are now pushed below normal levels. So your body responds by upregulating them. And that upregulation of androgens and sebum can, unfortunately, persist even after you stop the medication, resulting in higher androgen and sebum than you ever had before. And therefore the classic post-pill acne that typically begins about three months off the pill.
The same post-pill androgen surge can cause or worsen weight gain, as I mentioned, and also hair loss. Again, not instantly, but hair loss usually starts about 3 or 4 months after stopping the pill. And post-pill hair loss is a little more complicated in that it’s not always about androgens but can simply be the result of losing the pill’s estrogen, similar to what happens three months after having a baby. That kind of temporary hair loss is called telogen effluvium, whereas hair loss from androgens is called androgenic alopecia or female pattern hair loss. But to complicate things even more, a sudden exposure to androgens (such as from coming off a drospirenone pill) can cause telogen effluvium which then develops into androgenic alopecia. Other factors that affect hair include stress, illness, thyroid disease, low-carb diets, and nutrient deficiency, especially iron deficiency. So, to figure out what’s going on with your hair, you might need to do a little detective work with the help of your doctor.
So, what is the solution? Of course, one solution is to go back on an androgen-suppressing medication such as spironolactone. Which is basically the same drug as drospirenone and so, can help, of course. But, unless you plan to stay on it forever, you’ll eventually need to withdraw from spironolactone as well. So, through my lens, it’s better to just get the withdrawal process over with. While getting support from some of the natural treatments I’m now going to list. Preferably starting treatments before you stop the pill because it’s easier to prevent post-pill androgen symptoms than it is to treat them. And you’ll need to stick with the treatments because it can take at least six months to see results.
The first treatment for post-pill acne and other androgen symptoms is zinc. It works for skin because it’s antimicrobial; plus, for androgen symptoms generally, it downregulates the enzyme 5-alpha-reductase, thereby reducing DHT, which is the active form of testosterone. I generally recommend 30-50 mg of zinc to be taken directly after your biggest meal. Don’t take zinc on an empty stomach because it can make you feel sick.
The next strategy for skin, in particular, is to temporarily avoid the dairy protein A1 casein plus avoid concentrated sugars, especially soft drinks and fruit juices. Both dairy and concentrated sugar can worsen skin via several mechanisms including by spiking the hormone IGF-1. The good thing about diet changes for skin is that you usually only need to commit to them for six to twelve months until your skin clears. After that, you can probably get away with some dairy and sugar.
Next is the phytonutrient berberine, which also lowers IGF-1 and can be great for skin. Furthermore, berberine is antimicrobial and can help to reverse insulin resistance and lower androgens. Be careful with berberine because it’s not safe in pregnancy and has a few other contraindications. Best to check with your clinician or pharmacist before trying it.
Next is diindolylmethane or DIM which is a phytonutrient derived from vegetables such as broccoli. Taken as a supplement and at a dose of about 100 mg, DIM can help to block androgen receptors and improve post-pill acne. It’s very popular for skin.
Finally, myo-inositol or just inositol is the most researched supplement for androgen excess and PCOS. At a dose of 2 to 6 grams per day, inositol has been found to lower androgens. It works by improving insulin sensitivity and amplifying the FSH signal inside the ovarian follicle. Which means, of course, that inositol promotes ovulation.
Which brings us to the oh-so-important strategy of trying to establish regular ovulation because ovulation is how you make the best anti-androgen treatments: which are, of course, your own hormones estrogen and progesterone. You can also take progesterone, which we’ll talk about in a minute. But if you’re younger than 40, you should be able to make lots of progesterone on your own, as long as you’re able to ovulate. And remember, it’s possible to have somewhat regular periods but not be ovulating or making progesterone because you’re having anovulatory cycles. See the link in the show notes to my ovulation blog post.
If you figure out that you’re not ovulating, then your first stop is to see your doctor who will hopefully do some investigations and not just recommend going back on the pill. Her investigations should help to rule out or identify various possible obstacles to ovulation including high prolactin, thyroid problems, gluten sensitivity, nutrient deficiency, undereating, or PCOS, just to give some examples. Depending on which of those conditions is your diagnosis, your best strategy for regaining ovulation and therefore improving your post-pill androgen symptoms is to treat that condition. Keeping in mind that undereating could be your diagnosis even if you’ve been mistakenly told you have PCOS. Again, see episode 3.
If your diagnosis is PCOS and you’re confident in that diagnosis, you can look at PCOS treatments such as inositol which we discussed, as well as cyclic progesterone therapy. I’ve actually written a couple of peer-reviewed papers about cyclic progesterone therapy, which I’ll link to in the show notes, along with a blog post. It basically involves taking natural or body-identical progesterone for two weeks, then stopping it for two weeks and repeating that for at least three cycles, and maybe six cycles. Progesterone reduces androgens via several mechanisms including by lowering the hormone LH, as well as by competing for 5-alpha reductase and thereby lowering DHT. In that way, progesterone can improve all androgen symptoms including acne, hair loss, and weight gain. It can also promote regular ovulation which means you can then make your own progesterone and stop taking progesterone. Depending on your country, natural progesterone is available as the brands Prometrium or Utrogestan.
In closing, I’ll just acknowledge that post-pill androgen symptoms are tough to treat. You will likely get some relief from the treatments discussed, but you’ll also need to play the long game and know that after a year, you should be through the worst of the withdrawal process. And if you truly have PCOS, and not just a temporary post-pill androgen surge, you’ll likely need ongoing support, such as diet, zinc, and inositol.
I hope that’s been helpful and thanks so much for listening. Please share and leave a review. And I’ll see you next time when I’ll do a deeper dive into the supplement myo-inositol.
