A tendency to allergies or high histamine can increase the risk of perimenopausal symptoms such as night sweats, anxiety, pain, sleep disturbance, migraines, and heavy periods. That’s because histamine increases with estrogen, and estrogen is higher than normal during the early years of perimenopause.
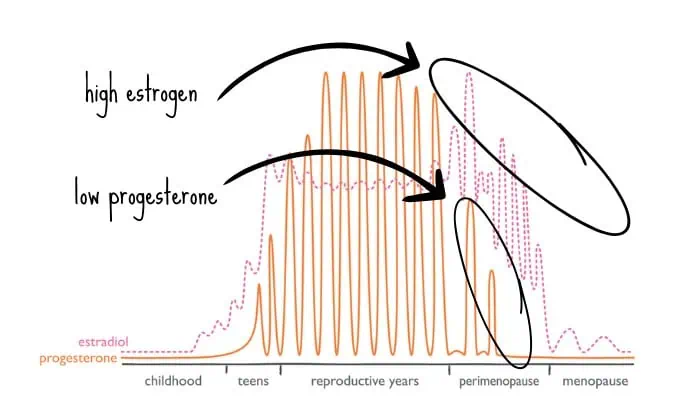
Estrogen goes up before it goes down
During perimenopause, estrogen starts to fluctuate more widely and soar every month to above-normal levels—only to crash down again to a low-level baseline.
Crashing or falling estrogen causes “estrogen withdrawal.” That’s one driver of the neurological symptoms of perimenopause. Another major driver is high histamine or mast cell activation from the spikes of very high estrogen. (Mast cells are the immune cells that release histamine.)
Histamine is a stimulating neurotransmitter
High histamine causes neurological symptoms because histamine is not just an immune or inflammatory mediator—it’s also a stimulating neurotransmitter that promotes alertness and wakefulness. (That’s why antihistamines are sedating.)
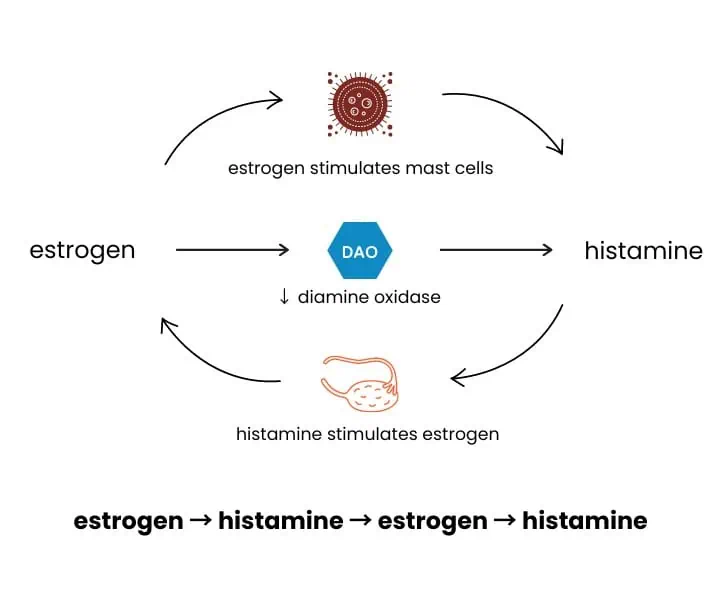
How estrogen increases histamine
High estrogen causes high histamine via three key mechanisms:
- Mast cell activation: Estrogen activates mast cells, prompting them to release stored histamine and heparin, which is a blood thinner. That’s why mast cell activation can cause or worsen heavy menstrual flow.
- Histidine decarboxylase expression: Estrogen boosts the expression of histidine decarboxylase, the enzyme that converts histidine to histamine.
- DAO enzyme downregulation: Estrogen downregulates the DAO enzyme, which is responsible for clearing histamine.
At the same time, in the other direction, histamine stimulates the ovaries to make more estrogen. The net result can be a vicious cycle of estrogen causing high histamine, causing high estrogen, causing even more histamine.
Losing progesterone
Progesterone should normally keep histamine in check by stabilizing mast cells and upregulating DAO. Unfortunately, progesterone drops early in perimenopause, so cannot exert its normal antihistamine effect.
👉🏽 Tip: The progestins of hormonal birth control do not have the same beneficial antihistamine effect as progesterone.
Recognizing high histamine symptoms
Symptoms of high histamine include:
- urticaria or hives
- fluid retention
- tinnitus or ringing in the ears
- anxiety or agitation
- insomnia
- brain fog
- headaches, especially migraines, and
- breast tenderness.
As you can see, symptoms of high histamine are quite similar to symptoms of perimenopause. Of course, high histamine is not the only cause of those symptoms, but it is a cause and a fairly easy one to address.
Strategies to lower histamine and relieve symptoms of perimenopause
- Reduce histamine-containing foods, especially wine, which has a high histamine content.
- Identify and avoid food sensitivities, such as cow’s dairy, because they can activate mast cells and release histamine.
- Support methylation with supplements like B vitamins, choline, and SAM-e to promote the healthy breakdown of histamine via the enzyme Histamine N-methyltransferase.
- Address gut health by treating underlying issues like SIBO that can exacerbate mast cell and histamine problems.
- Consider natural antihistamine supplements such as quercetin, which stabilizes mast cells, and vitamin B6, which upregulates the DAO enzyme. (But be careful with the dose of vitamin B6.)
- Use antihistamine medication. (Long-term use of antihistamines can increase the risk of cognitive decline, but short-term use is fine.)
- Try body-identical progesterone, which can counterbalance high estrogen and relieve histamine symptoms.
Have you had relief from an antihistamine approach? Share your story and strategies in the comments.
For further reading, refer to the histamine sections in my books about periods, hormones, and metabolism.