Progesterone is usually soothing to mood but can sometimes cause anxiety.
A negative mood reaction to changing levels of progesterone is called neurosteroid change sensitivity or premenstrual dysphoric disorder (PMDD) and affects about one in twenty women.
Also, see Top 6 natural treatments for premenstrual mood symptoms.
Contraceptive progestin drugs are bad for mood
Progestins are not the same as the body’s own progesterone, so should not come into this conversation. Unfortunately, many doctors, journalists, and even scientists confuse progestins with progesterone and say, “progesterone is bad for mood,” when they really mean progestins are bad for mood.
Contraceptive progestins such as levonorgestrel, drospirenone, and norethisterone have all been linked with anxiety and depression, but mood symptoms from birth control are drug side effects, not PMS or PMDD.
Progesterone and the brain
For most women, progesterone is good for mood because it converts to a neurosteroid called allopregnanolone, which calms GABA receptors. Progesterone’s calming neurosteroid effect is why progesterone capsules are usually sedating and why women can feel drowsy during times of high progesterone, such as the early luteal phase and pregnancy. Progestins do not convert to allopregnanolone, so progestins cannot soothe mood like progesterone can.
For women with PMDD, allopregnanolone does not calm GABA receptors but instead can stimulate them in a way that produces anxiety and other negative mood symptoms. It’s not that women with PMDD have more allopregnanolone; in fact, they may have less. Instead, their GABA receptors seem to have an abnormal response to allopregnanolone.
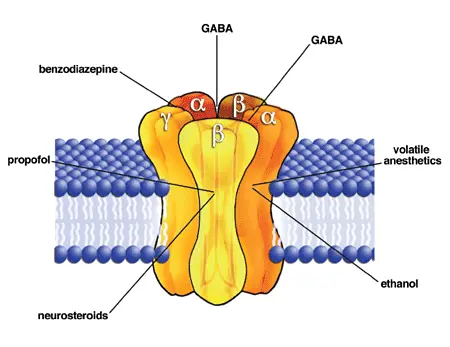
GABA receptors consist of five subunits that reshuffle and change configuration to adapt to the normal ups and downs of allopregnanolone. With PMDD, the GABA receptors are less able to adapt to changing levels of allopregnanolone. The result, according to researcher Tory Eisenlohr-Moul, is neurosteroid change sensitivity and the mood symptoms of PMDD.
Another potential factor is that progesterone can cause intestinal permeability, leading to high LPS endotoxin and negative mood symptoms. According to the research, an underlying tendency to progesterone deficiency increases the risk of this negative endotoxin effect on mood.
Conventional treatment of PMDD
Conventional treatment for PMDD includes:
- SSRI antidepressants to modulate GABA receptors and/or
- hormonal birth control to shut down ovulation and progesterone.
The problem with this approach is that:
- SSRI antidepressants may increase the risk of osteoporosis.
- Contraceptive progestin drugs carry their own set of mood side effects.
- Women need ovulation and progesterone for long-term health. According to Professor Jerilynn Prior, “regular menstrual cycles with consistently normal ovulation [and progesterone]…will prevent osteoporosis, breast cancer and heart disease.”
How to take progesterone for premenstrual mood symptoms
The better approach is to stabilize GABA receptors and, therefore, be able to tolerate the normal ups and downs of progesterone.
It’s also possible to take progesterone. For women with mild premenstrual symptoms (PMS instead of PMDD), low-dose progesterone (such as progesterone cream) can relieve premenstrual mood symptoms by relieving the “progesterone withdrawal” or “GABAergic withdrawal” that occurs at the end of the cycle.
For women with neurosteroid change sensitivity and PMDD, a higher dose of progesterone (200 mg) can work better than a lower dose. That’s because of the bimodal association between serum allopregnanolone and adverse mood, which means that, for women with PMDD, normal endogenous levels of progesterone can be anxiety-provoking, but above-endogenous levels (such as 200 mg) can be calming. Unfortunately, very high doses above 400 mg are likely to cause depression in anyone, and unfortunately, the few studies of progesterone for premenstrual mood all used very high doses of 400 to 1200 mg.
Natural treatment of PMDD
As I discuss in my summary blog post and podcast/YouTube video about premenstrual mood symptoms, other treatment strategies include:
- Reduce histamine and mast cell activation, which relieves histamine-induced mood symptoms and may normalize the sensitivity of GABA receptors. Histamine is one aspect of chronic inflammation and a known driver of premenstrual mood symptoms. For more, read The role of histamine and mast cells in PMS and PMDD.
👉 Tip: For many of my patients, avoiding cow’s dairy is the fastest way to reduce a mast cell or histamine reaction. Avoiding A1 casein (and its inflammatory opioid peptide BCM7) can also improve GABA levels.
- Take magnesium, which supports a healthy GABA response and relieves PMS by “normalizing the action of progesterone on the central nervous system.” The best form is magnesium glycinate or bisglycinate because the amino acid glycine also calms GABA receptors.
👉 Tip: The therapeutic dose is 300 mg of elemental magnesium, so read the label carefully. Most magnesium capsules contain 100 mg.
- Vitamin B6 (pyridoxine) has performed well in at least one clinical trial for PMDD. It works by boosting GABA, lowering prolactin, and promoting the healthy clearance of histamine. Be careful with vitamin B6 because it can cause nerve damage.
👉 Tip: I get the best results with magnesium, vitamin B6, and the amino acid taurine (because taurine calms GABA receptors).