Perimenopause, or “second puberty,” is the two to ten years before the final period. It’s different from menopause (or post-menopause), which is the life phase that begins one year after the final period. Symptoms can occur during perimenopause and are temporary.
Your final period (menopause) could be anywhere from age 45 to 55, so perimenopause could start as young as your late 30s, but more likely your mid-40s. That means you could be in the territory of perimenopause if you were born before 1986—still relatively young. That’s why perimenopause is not about aging. Instead, it’s an important (and unavoidable) recalibration of your hormonal and nervous systems.
The timing of menopause is genetic
As I explain in my book Hormone Repair Manual, menopause has been around for as long as we’ve been human and is not an accident of living too long. In fact, according to some historians, menopause may have been the driving force behind the evolution of a longer human lifespan.
You are genetically programmed to achieve menopause (periods completely stopped) approximately when your mother or female relatives achieve it. If that’s on the younger end of normal (mid-40s), that’s just how you are. It doesn’t mean you’re aging more rapidly than your friends. If, on the other hand, you’re genetically programmed to achieve menopause on the older end of normal (mid-50s), perimenopause is happening alongside aging but is not caused by aging.

Finally, if you achieve menopause before age 40, it’s the medical condition of premature menopause or primary ovarian insufficiency (POI) and is also not about aging.
How to diagnose perimenopause
Menopause or post-menopause (including early menopause) can be diagnosed by two high FSH readings (more than 40 IU/L) at least a month apart.
Perimenopause cannot be diagnosed by FSH or any other lab test. Instead, it’s diagnosed based on age and symptoms. According to Canadian endocrinology professor Jerilynn C Prior, a midlife woman with regular cycles is likely to be in perimenopause if she notices any three of the following nine changes:
- new-onset of heavy and/or longer flow
- shorter menstrual cycles (<26 days)
- new sore, swollen or lumpy breasts
- new mid-sleep waking
- increased menstrual cramps
- premenstrual night sweats
- new or markedly increased migraine headaches
- new or increased premenstrual mood swings
- weight gain without changes in exercise or eating.
In other words, if you’re older than 37 and have at least three symptoms on this list (and other explanations have been ruled out), you’re likely to be in perimenopause.
What are the hormonal changes of perimenopause?
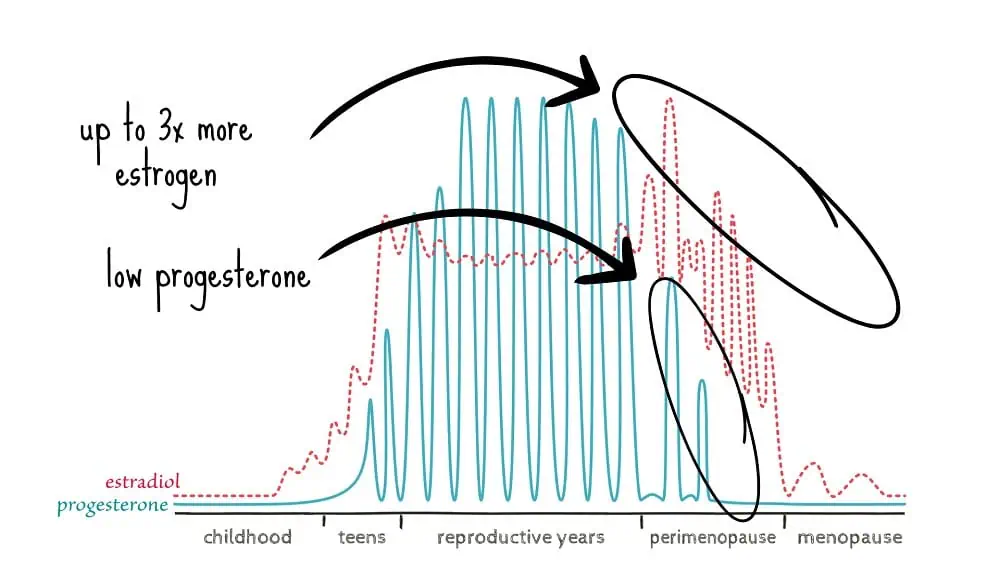
During perimenopause, the first hormonal change is a drop in progesterone, thanks to shorter luteal phases and more anovulatory cycles—despite still having regular periods. Losing progesterone can contribute to anxiety, breast pain, heart palpitations, night sweats, frequent migraines and crazy, heavy periods.
Just as progesterone starts to drop away, estrogen starts to spike up to three times normal. And that can contribute to irritable mood, breast pain and heavy periods.
👉🏽 Tip: High estrogen stimulates mast cells and histamine, which can contribute to symptoms like insomnia, breast pain, and heavy periods.
The fact that perimenopausal symptoms stem largely from losing progesterone, not estrogen, is why progesterone, not estrogen, can be the better treatment. And just a little reassurance: it is possible to conceive during perimenopause.
For treatment ideas, see my book Hormone Repair Manual, where I discuss my favourite combo of magnesium, taurine, and modern body-identical hormone therapy, including transdermal estrogen (Estradot) and natural progesterone (Prometrium or Utrogestan).
Further information:
- What estrogen does in your 40s and how progesterone can help
- Natural treatment of heavy periods
- Why I prescribe iodine for breast pain, ovarian cysts, and PMDD
- The role of histamine and mast cells in PMS and PMDD