Progesterone has been both ignored and wrongly blamed for side effects it does not cause. How did that happen?
For one thing, progesterone was discovered shortly after estrogen. Thus missing the opportunity to be part of the tidy hormone dichotomy of “testosterone for men and estrogen for women.” Also, progesterone could not (at first) be made into an oral medication, so was replaced by progestins.
For example, while early preparations of testosterone (testosterone propionate, 1940s) and estrogen (estradiol valerate, 1960s) were body-identical or natural hormones, body-identical progesterone (oral micronized progesterone) didn’t become available until the 1990s.
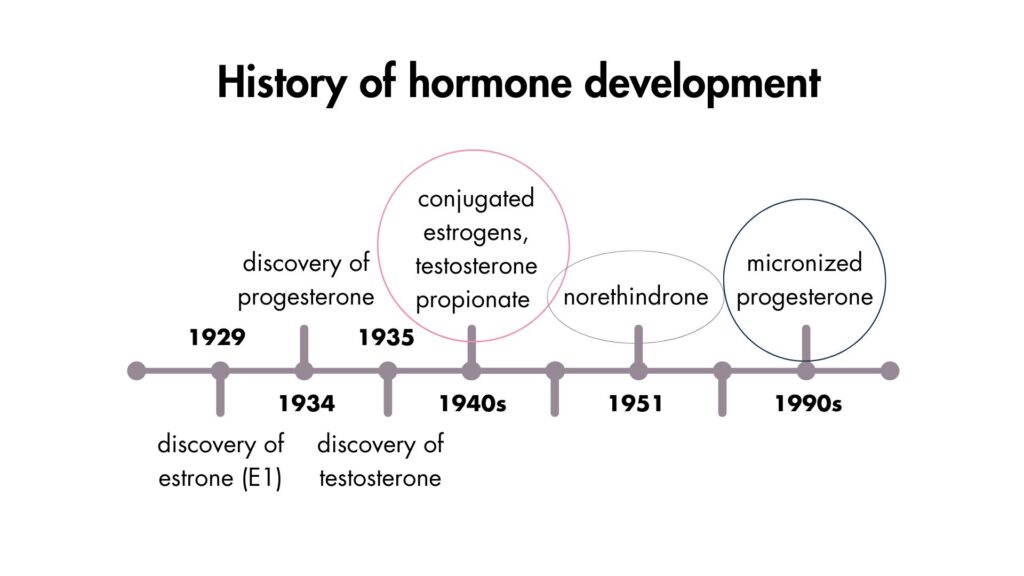
For decades, synthetic progestins were used in research and treatment, but, unfortunately, progestins have different (and sometimes opposite) effects than progesterone.
👉🏽 Did you know? Estrogen is a generic term that encompasses both ovarian estradiol and synthetic compounds like ethinylestradiol. In contrast, progesterone refers exclusively to the natural hormone progesterone and does not include synthetic progestin.
Sadly, many of the side effects and risks of progestins have been mistakenly attributed to progesterone. For example, progestins increase the risk of breast cancer, but progesterone reduces it.
After decades of dismissing body-identical progesterone, experts now agree it’s safer than progestins. The evidence was always there.
Estrogen and progesterone work together to build long-term health
It’s time to bring real progesterone (not progestins) back into the conversation because estradiol (estrogen) and progesterone work as a team. For example, the pre-ovulatory surge of estradiol promotes healthy ovulation and the release of progesterone. Estradiol also upregulates progesterone receptors.
In turn, progesterone counterbalances estradiol in every part of the body, including:
- the uterus, where progesterone thins the lining while estradiol thickens it
- the brain, where progesterone calms the brain while estradiol stimulates it
- the breasts, where progesterone slows cell division while estradiol increases it.
Progesterone also provides important feedback to the brain to promote healthy ovulation in the subsequent cycle.
👉🏽 Did you know? On a blood test, a good peak luteal phase progesterone level is 80 nmol/L, 100 times more than an average peak estradiol level of 800 pmol/L (0.8 nmol/L).
Together, estrogen and progesterone promote the long-term health of the brain, bones, and cardiovascular system. In the words of Professor Prior, “Ovulatory cycles across a woman’s long reproductive life span are needed to prevent osteoporosis and fracture, heart attacks, and breast and endometrial cancers during women’s older years.“
Every ovulatory cycle is like a deposit into the bank account of long-term health.

Do you make progesterone?
A regular ovulatory menstrual cycle is the only way to make progesterone.
Definition: An ovulatory cycle is a menstrual cycle in which ovulation occurs and progesterone is made.
A cycle without ovulation or progesterone is called an anovulatory cycle and is common. Read Ovulation is the main event of the menstrual cycle.
💡Tip: Knowing if and when you ovulate is called body literacy.
For more, see:
- My books Period Repair Manual and Hormone Repair Manual
- A safer type of hormone therapy
- The right way to test progesterone
- Roadmap to progesterone
- Guide to using progesterone for women’s health